Bronchoaspiration in older adults
¿What happens to the patient?
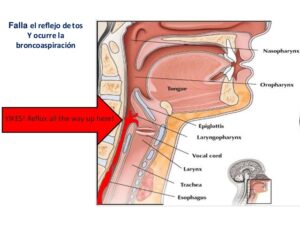
Bronchial aspiration consists of the accidental aspiration of solids or liquids through the airway. It can also occur in unconscious people or in babies so that the food is accumulated in the mouth and is carried towards the bronchial tubes at the time of inhaling what obstructs the respiratory tract.
Causes of aspiration
- Bronchial aspiration can occur as a result of conditions that leave the patient in a state of unconsciousness or unable to move.
- It also often happens with babies, or with young children, since they commonly put everything they find at hand in their mouths. Especially when it comes to small things that can obstruct the airways and cause suffocation if they are not expelled in time.
Symptoms of aspiration
- Difficulty breathing.
- Cough.
- Stridor, that is, noises when breathing in.
- Cyanosis (purple discoloration of the skin).
- In extreme cases in which the situation is sustained over time and oxygen deprivation is very important, loss of consciousness occurs.
Prevention
Prevention of aspiration during feeding by mouth
- Let the patient rest for 30 minutes before feeding time; if you are rested, the person is likely to have less trouble swallowing.
- The person must be upright in a chair; if bedridden, the backrest should be raised to a 90-degree angle.
- Tipping your head slightly with your chin down will help reduce aspiration in some types of dysphagia.
- Adjust the rate of feeding and the size of the bites according to the person’s tolerance and avoid rushed or forced feeding.
- Alternate solid and liquid boluses.
- Introduce the food into the patient’s mouth according to the type of deficit. For example, feeding can be given on the right side of the mouth if there is facial weakness on the left side.
- Determine the viscosity of the food that is best tolerated by the person. Example: Some people swallow thick liquids more easily than thinner liquids.
- According to a recent study, higher food viscosity markedly improved
swallowing ability in neurological patients. This means that aspiration was significantly reduced when patients swallowed juice or pudding (compared to swallowing liquids). - Minimize the use of sedatives and sedative-hypnotics as these agents can affect the cough reflex and swallowing.
- Assess the effectiveness of techniques such as cueing, redirection, task segmentation, and environmental modifications (to minimize distractions) as alternatives to mouth feeding.

Prevention of aspiration during tube feeding
- People who aspirate food during oral feedings are likely to also aspirate during tube feedings, either through nasogastric or gastrostomy tubes.
- Therefore, the growing trend is to avoid the use of tube feeding solely for the purpose of avoiding aspiration.
- There are situations when tube feeding is necessary, especially during periods of acute illness.
When tube feeding is necessary, the following activities can help reduce aspiration:
- Keep the back of the bed elevated at least 30º during continuous feedings.
- When the tube-fed person is able to communicate, it is important to ask if they have any of the following symptoms of GI intolerance: nausea, feeling full, abdominal pain, and cramps.
- These symptoms are signs of slow gastric emptying which can, in turn, increase the likelihood of regurgitation and aspiration of gastric contents.
- Measure gastric residual volumes every 4 to 6 hours during continuous feedings immediately before each intermittent feeding.
- This evaluation is especially important when the tube-fed person is unable to communicate symptoms of gastrointestinal intolerance.
- Although there is no convincing research information regarding what is considered excessive gastric residual volume, a persistently elevated amount (eg, greater than 200 mL) should cause concern.
- A prokinetic agent (such as metoclopramide or erythromycin) may be given to relieve slow gastric emptying.
- Postpyloric feeding tube placement (jejunostomy) may be indicated if slow gastric emptying becomes a problem. There is controversy about the effectiveness of this option.
- Pump feeding may be associated with fewer cases of aspiration than controlled gravity feeding in bedridden patients with gastrostomy tubes.

Prevention of aspiration pneumonia through oral care
- Missing teeth or poorly fitted dentures predispose to aspiration by interfering with chewing and swallowing.
- Infected teeth and poor oral hygiene predispose to pneumonia after aspiration of contaminated oral secretions.
- The results of a recent study suggest that tube feeding in older people is associated with significant pathogenic colonization of the mouth, even more so than that observed in people who were fed by mouth.
- Evidence indicates that weekly dental care and cleaning the older person’s teeth with a toothbrush after every meal reduces the risk of aspiration pneumonia.

Treatment
- Treatment of aspiration is to focus on clearing the patient’s airway to restore normal respiratory function.
- The object or substance that obstructs the pathways will be removed with sufficient care so that said element does not penetrate further into the interior.
- If it is an object, the most appropriate thing is to perform first aid maneuvers such as the Heimlich maneuver or CPR.
- If what obstructs the pathways is a liquid, the most convenient thing will be to perform a suction with a suction device and a probe appropriate to the patient and the process that we are going to carry out.
We must always bear in mind that even if the obstruction is partial and the patient has good respiratory function, the liquid or object, no matter how small, must be removed to avoid future complications.

Care plans
1.- Ineffective airway clearance secondary to suppression of the cough reflex.
Activities:
– Make postural changes.
– Respiratory physiotherapy (deep breaths, clapping, vibrations and forced expirations).
– Keep the patient hydrated to facilitate the expulsion of secretions.
2.- Ineffective respiratory patterns secondary to mechanical obstruction and pain.
Activities:
– Assess pain with the VAS scale to ensure patient comfort.
– Aspiration of secretions with a probe in intubated or tracheostomized patients.
3.- Impaired gas exchange secondary to general or spinal anesthesia and aspiration.
Activities:
– Maintain a patent airway by suctioning secretions or placing a mayo tube, if necessary.
– Maintain the patient’s oxygenation by monitoring O2 saturation, placing the pulse oximeter and checking that the alarms are properly set.
– Place the patient in an optimal position for oxygenation (35-45º).
– High Fowler’s position to facilitate maximum chest expansion.
4.- High risk of bronchial aspiration secondary to a decreased level of consciousness
Activities:
– Assess gastrointestinal function to rule out hypoactive peristalsis.
– Place the patient at 30º to avoid gastric reflux.
– Maintain the patency and function of nasogastric suction devices to prevent the accumulation of gastric contents.
– Provide frequent oral care to prevent colonization of the oropharynx with bacteria and inoculation of the lower airways.
– Treat nausea quickly.
I recommend the following article: ¿What equipment is in an Intensive Care Unit?
Bronchoaspiration in older adults
Author Information
- Enfermeria Buenos Aires
- Lorena Plazas, graduate in nursing. Own job
- https://pxhere.com
Last update: [08/02/2022]